Autoregulation monitoring after traumatic brain injury
Cerebral autoregulation is the mechanism that describes the stability of cerebral blood flow with changes in cerebral perfusion pressure (or arterial blood pressure). After trauma, cerebral autoregulation can be impaired, leaving the brain vulnerable to further insults (Engelborghs et al., 2000). Cerebral autoregulation can be assessed in the brain trauma population using transcranial doppler (Mean flow index – Mx), near infrared spectroscopy (Total oxygenation reactivity index – TOx), brain tissue oxygenation (Oxygen reactivity index – ORx), or even intracranial pressure monitoring (pressure reactivity index – PRx).
Disturbed autoregulation as measured with both Doppler and PRx are related to worse patient outcomes (Czosnyka et al., 1996, Czosnyka et al., 1997, Liu et al., 2015).
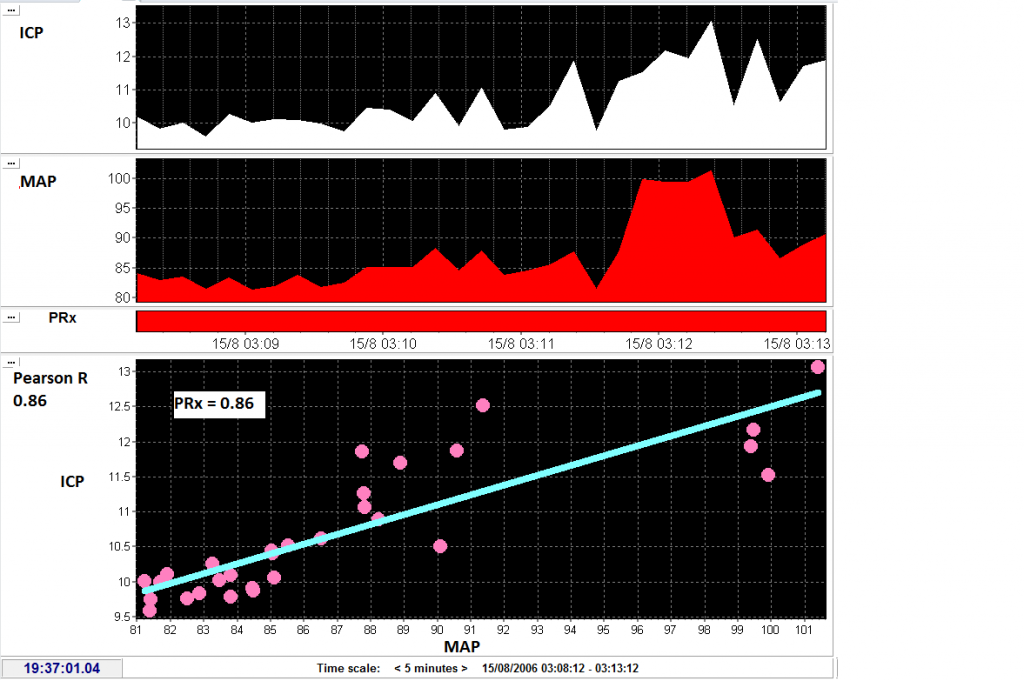
Pressure reactivity is calculated as the Pearson correlation between mean arterial pressure and intracranial pressure. Mean values of ICP and MAP are calculated every 10 seconds and then correlation of 30 consecutive values is taken. In this case variations in MAP occur with simultaneous changes in ICP and thus the PRx is impaired (close to 1). View image
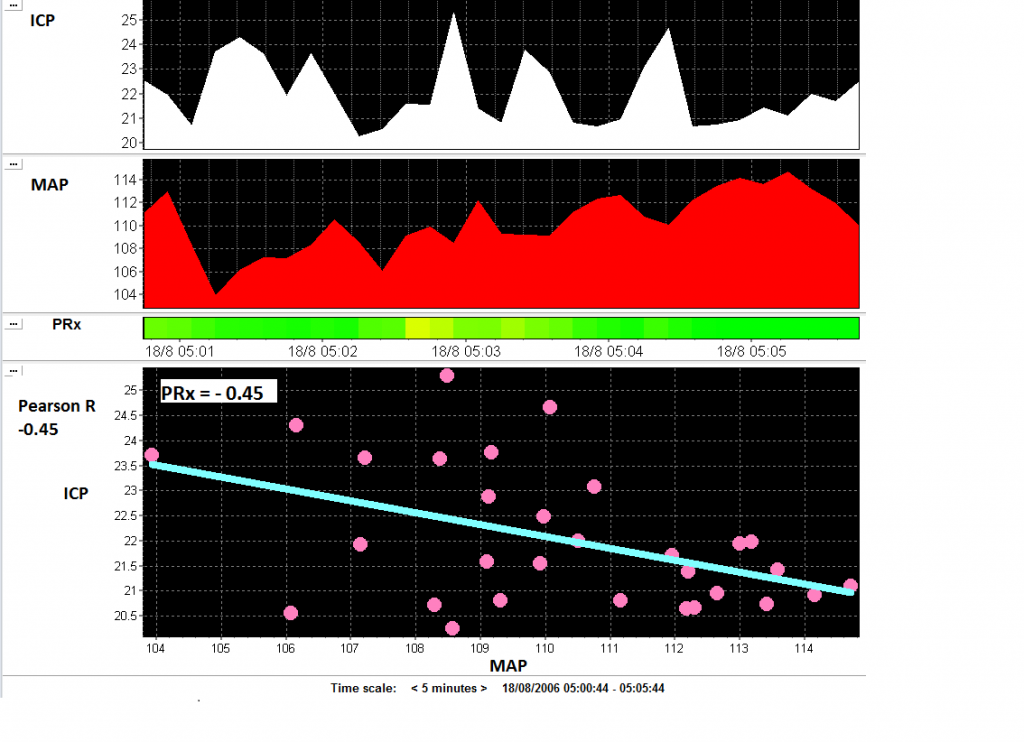
In cases when the brain vasculature is healthy, increases in MAP will be associated with decreases in ICP because an increase in MAP will cause cerebral vasoconstriction, decreased cerebral blood volume, and decreased ICP. The correlation between MAP and ICP will be negative (in this case PRx = -0.45). View image
Optimal CPP (CPPopt)
Cerebral perfusion pressure (CPP) is a major determinant of cerebral blood flow (reviewed in Donnelly et al., 2016) and can be modified in the intensive care unit by adjusting the dose of vasopressors. However, knowing which specific CPP is adequate for a patient after traumatic brain injury can be difficult – too low CPP risks ischaemia, whereas too high CPP risks lung and heart damage, as well as cerebral hyperaemia.
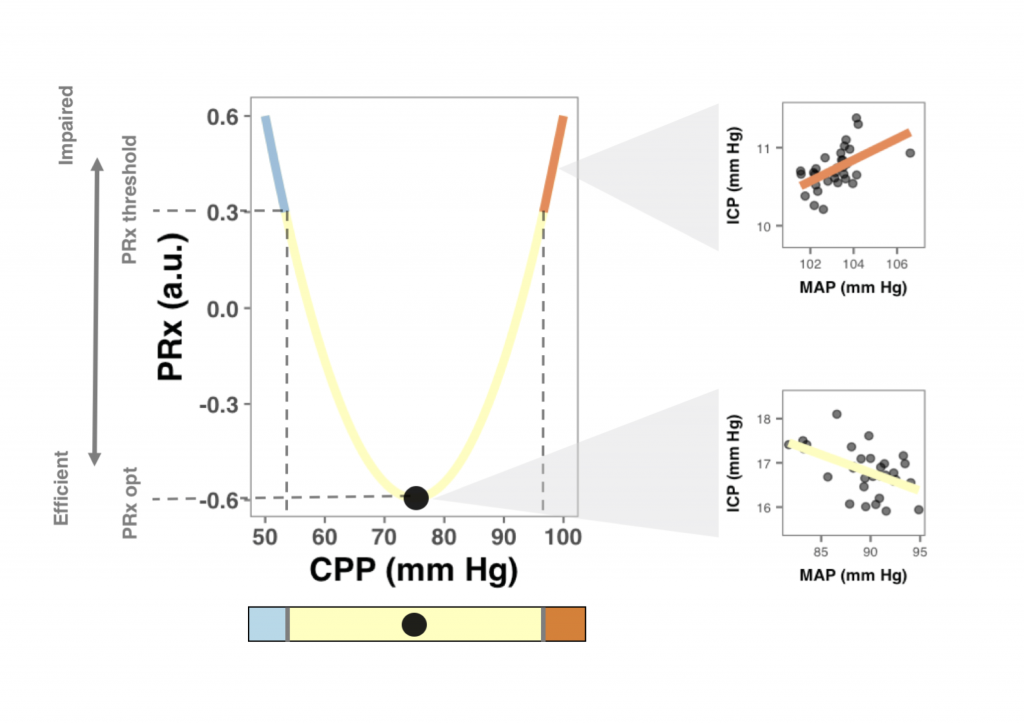
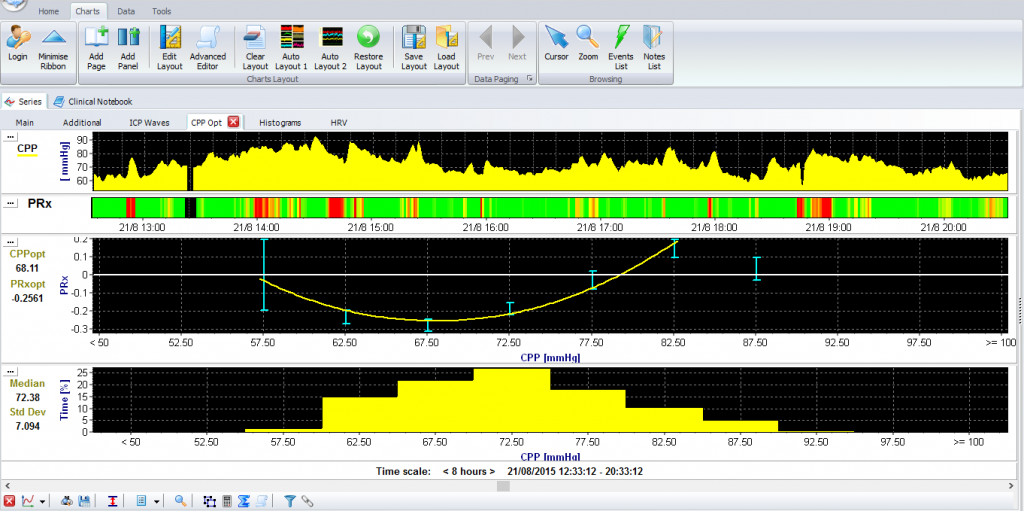
One method that has been proposed to find an individualised ‘optimal’ CPP (CPPopt) combines continuous monitoring of CPP and PRx (Steiner et al., 2002). In this way, the CPP at which the brain vessels react best is found (See explanatory figure below – full paper on journal website). This value may be different between patients, and may change in time within a patient (Aries et al., 2012). ICM+ allows for almost continuous estimation of CPPopt as well as estimated lower and upper CPP limits of pressure reactivity (Donnelly et al., 2017).
A randomised controlled trial of the feasibility of CPPopt therapy is currently being planned (www.cppopt.org, clinical trial number: NCT02982122)