Non-Invasive Intracranial Pressure analysis using ICM+
Intracranial pressure (ICP) is an important monitoring modality in the clinical management of several neurological diseases carrying the risk of fatal intracranial hypertension. However, this parameter is not always considered due to its invasive method of assessment. In this scenario, a non-invasive estimation of ICP (nICP) may be essential, and it has become a Holy Grail in Clinical Neurosciences.
Although ICP can guide patient management in neurocritical care, mainly traumatic brain injury (TBI), this is not commonly monitored in many clinical conditions outside of this environment. The invasive character of the standard methods for ICP monitoring and their associated risks to the patient (infections, brain tissue lesions, haemorrhage) contribute to this scenario. These drawbacks have prevented ICP monitoring in a broad range of diseases like in patients with risk of coagulopathy, as well as in other conditions, in which invasive monitoring is not considered or is outweighed by the risks of the procedure.
Provided that knowledge of ICP can be crucial for the successful management of patients in many subcritical conditions, nICP estimation of ICP may be helpful when indications for invasive ICP monitoring are not met, and when it is not immediately available or even contraindicated. Several methods for nICP assessment have been described so far: transcranial Doppler ultrasonography (TCD) to measure cerebral blood flow velocity indices, skull vibrations, brain tissue resonance, or transcranial time of flight, venous ophthalmodynamometry, optic nerve sheath diameter assessment (ONSD), sensing tympanic membrane displacement (TMD), otoacoustic emissions, magnetic resonance imaging to estimate intracranial compliance, ultrasound-guided eyeball compression, and recordings of visual evoked potentials. These methods are better suited for one-point assessment of the instant value of ICP rather than continuous monitoring.
Transcranial Doppler ultrasonography (TCD) was first described by Aaslid and collaborators in 1982. Apart from having many clinical applications, TCD waveform analysis has been investigated as a technique for nICP estimation, and this could represent one of its most useful applications outside of the critical care environment. It is conceivable if one considers that increased ICP could affect the waveform of blood flow velocity in major cerebral vessels which have compliant walls.
With ICM+, it is possible to explore various nICP formulae based on the data collected from TCD. TCD-based nICP methods rely on an approximate semi-quantitative assessment of relationship between cerebrovascular dynamics and ICP. They can be divided into three categories: I) methods based on the TCD-derived pulsatility index, II) methods based on the calculation of non-invasive cerebral perfusion pressure (nCPP), and III) methods based on mathematical models.
Some examples are depicted in this page.
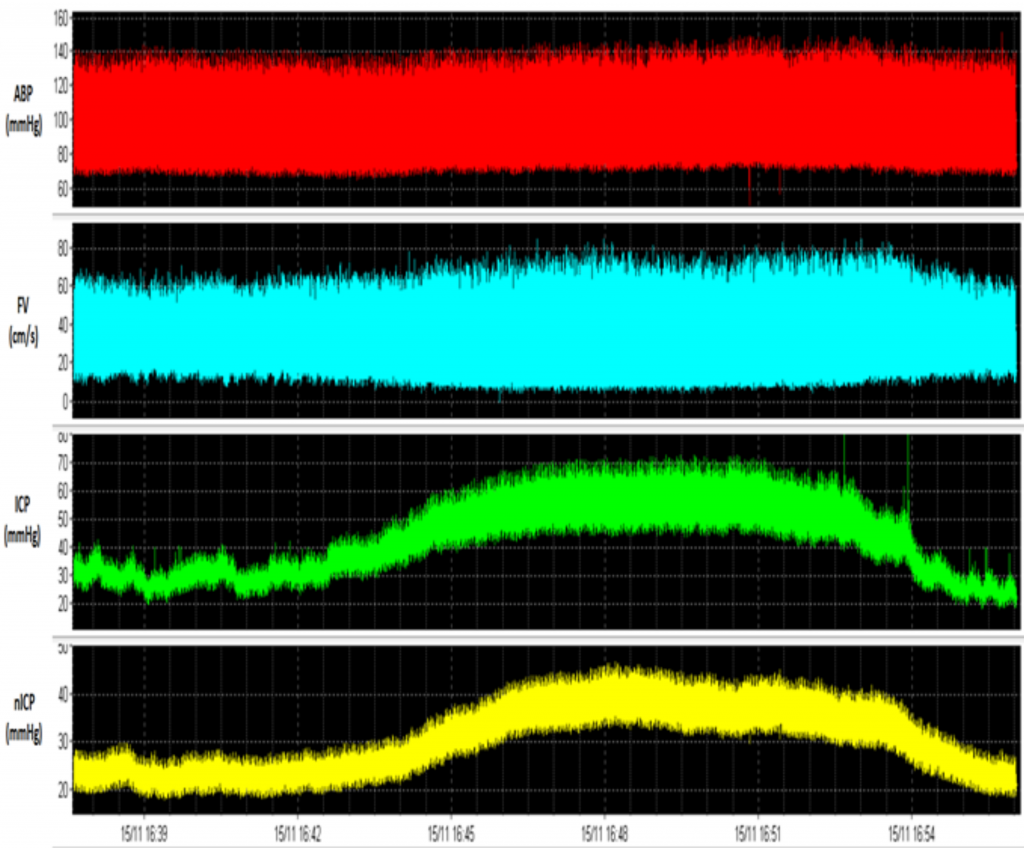
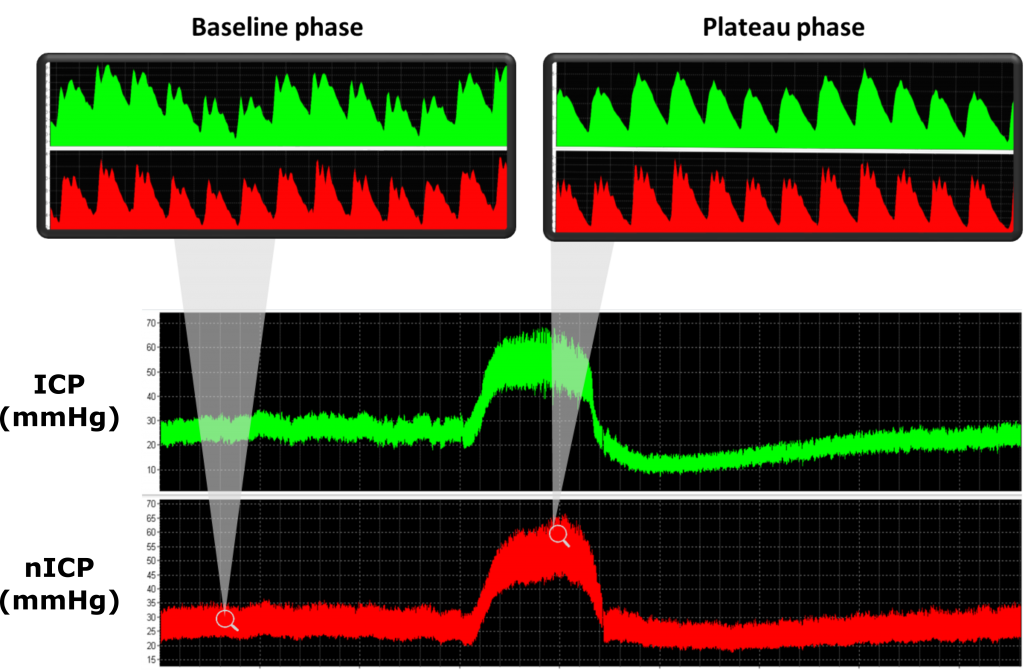
Example of a recording showing a raw data recording of arterial blood pressure (ABP, in mmHg), cerebral blood flow velocity (FV, in cm/s), invasive intracranial pressure (ICP, in mmHg) and non-invasive intracranial pressure (nICP, based on a black box mathematical model, in mmHg) during a plateau wave of ICP. Certain changes in FV, like a drop in the diastolic component, is observed during plateau waves.
Plateau waves of ICP (or Lundberg A-waves) are characterised by sudden and relevant increases in ICP (generally up to 40 mmHg), related to the increased volume of arterial blood in response to an arterial vasodilation stimulus. Such phenomena may develop in patients presenting intact cerebral autoregulation and low cerebrospinal compensatory reserve, suffering from a wide range of cerebral pathological conditions including TBI, idiopathic intracranial hypertension, subarachnoid haemorrhage, brain tumours, hydrocephalus, and craniosynostosis. View image
Different approaches for transcranial Doppler-based non-invasive ICP assessment
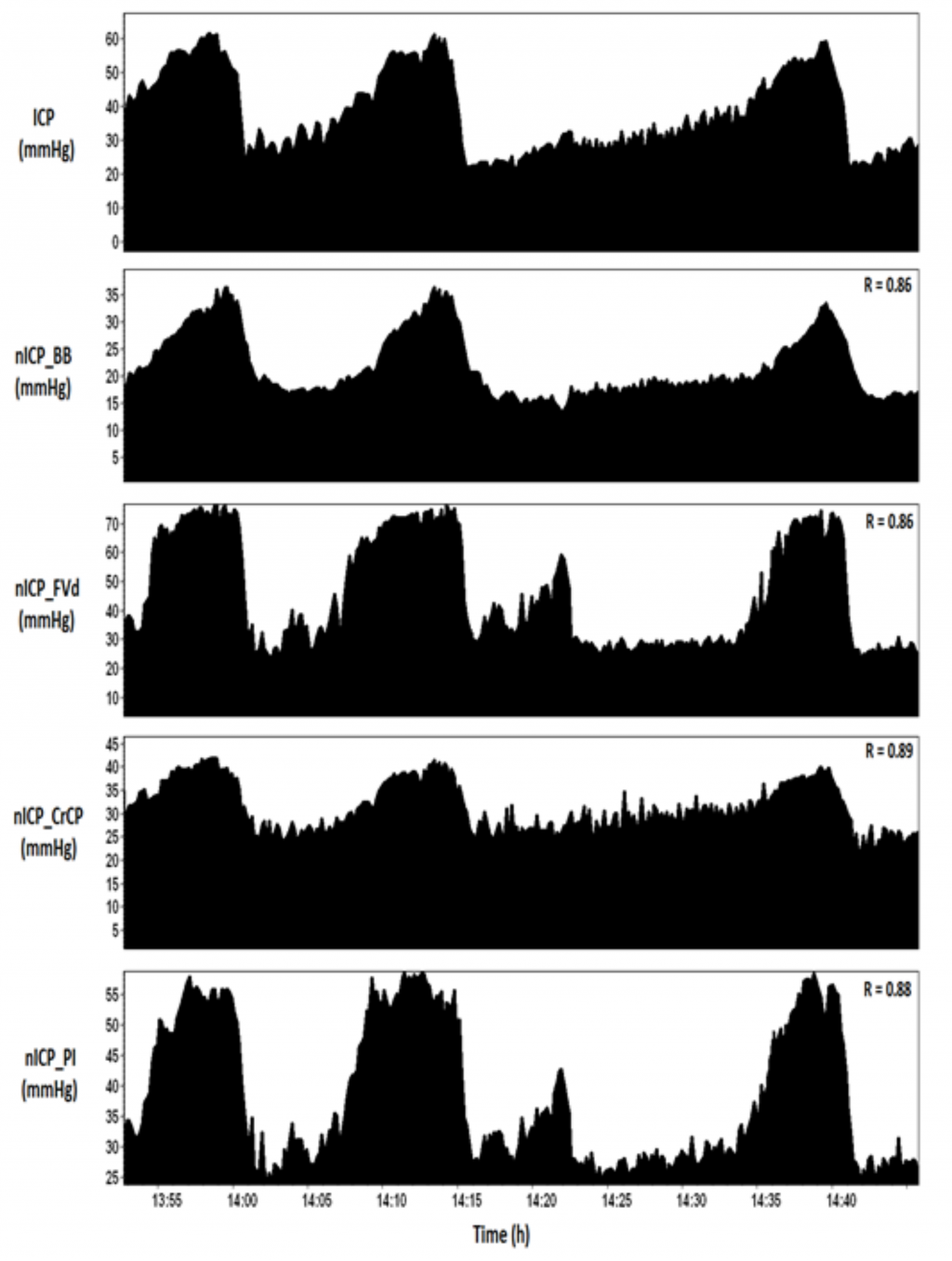
TCD-based nICP methods
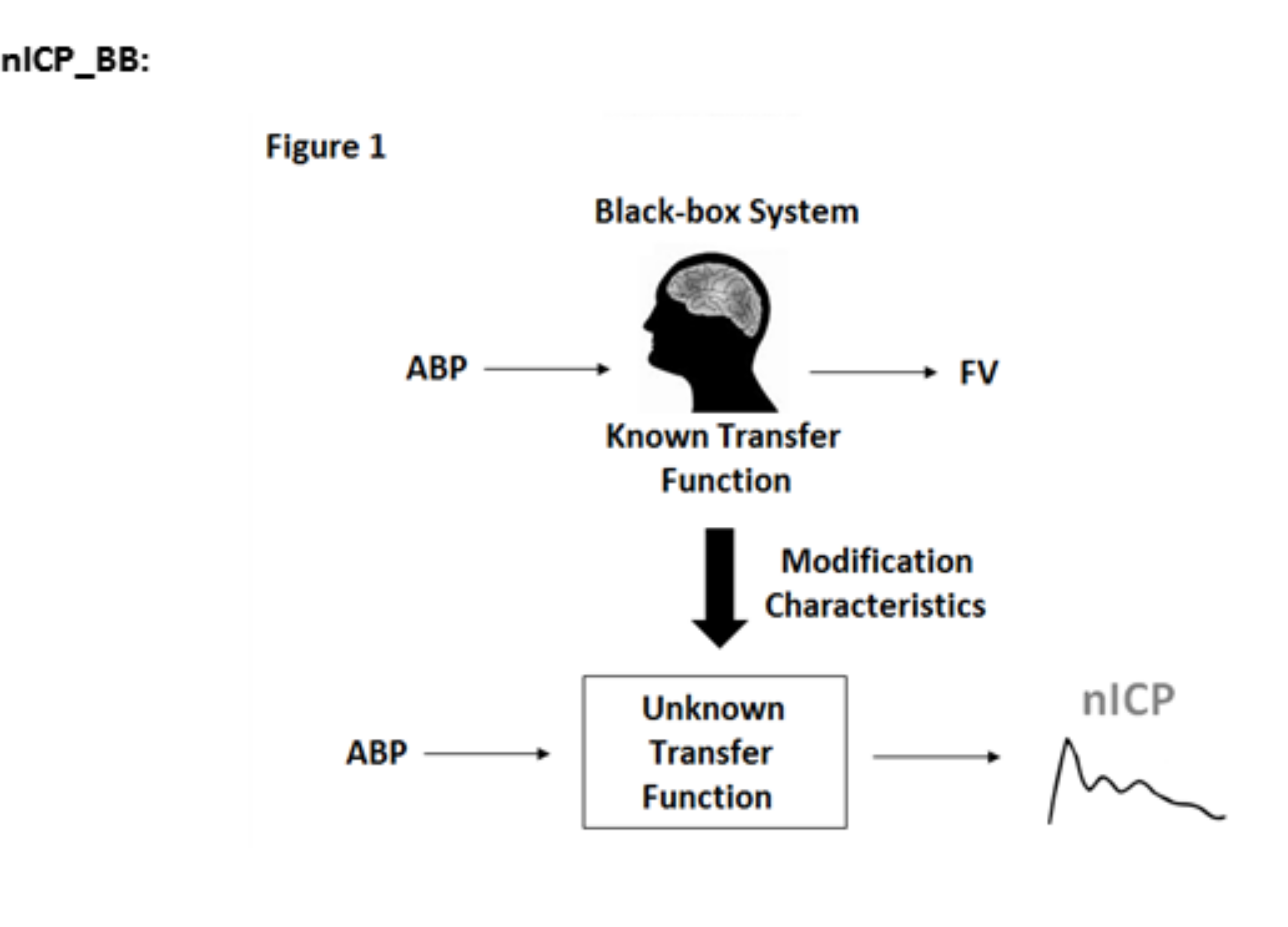
This method is described in terms of a transfer function between arterial blood pressure (ABP) and ICP, controlled by TCD and ABP derived parameters. The rules of this TCD-based linear control had been formerly determined using a multiple regression model between TCD parameters and ABP-ICP transfer function on datasets of reference patients. The model provides a full waveform of nICP (in mmHg). In ICM+, this model can be used via a plugin.
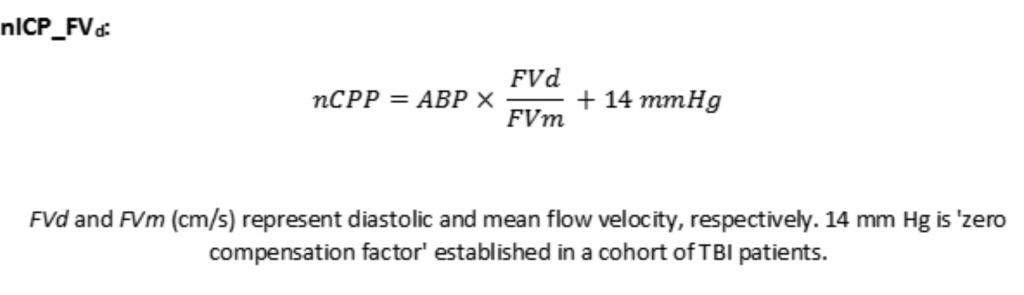
This method applies the diastolic flow velocity waveform analysis for the estimation of non-invasive cerebral perfusion pressure (nCPP). nICP can be calculated as the difference between mean ABP (ABPm) and nCPP (nICP = ABPm – nCPP). View image
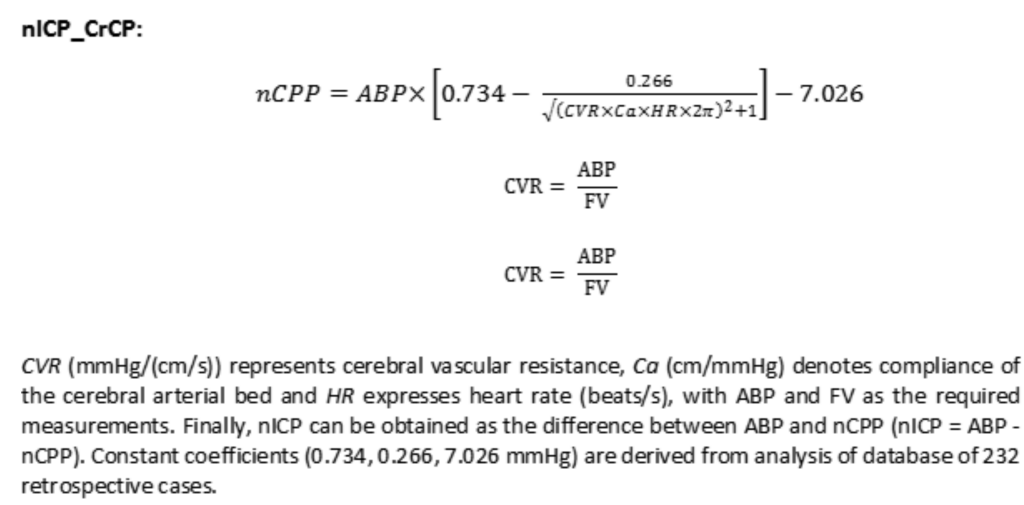
This method estimates nICP based on nCPP, in this case specifically using the concept of critical closing pressure (CrCP). CrCP denotes a threshold of ABP, below which the brain microvascular blood pressure is inadequate to prevent the collapse and cessation of blood flow. View image
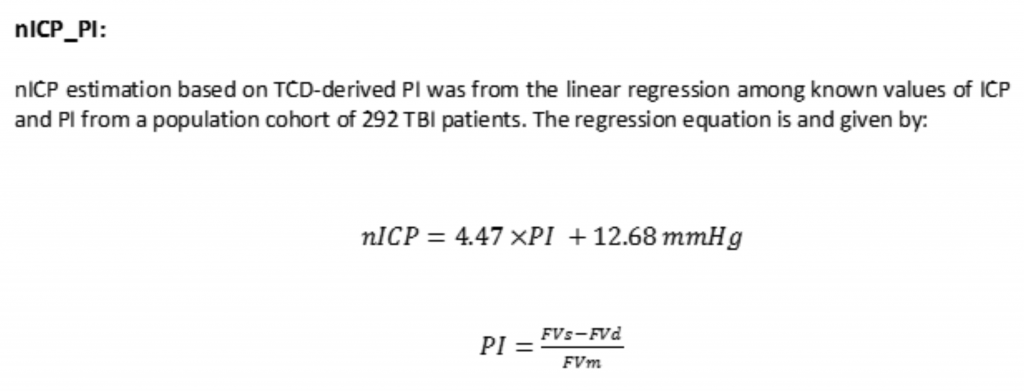
Pulsatility index (PI) describes changes in the morphology of the FV waveform. PI is a relationship between the difference of systolic (FVs) and diastolic (FVd) flow velocities divided by the mean flow velocity (FVm).
View image

